 Catherine saw me at eight weeks gestation for management of her 4th pregnancy. Her first three pregnancies had been unsuccessful.
Catherine saw me at eight weeks gestation for management of her 4th pregnancy. Her first three pregnancies had been unsuccessful.
She told me in her first pregnancy she had a placental abruption with threatened preterm labour at 23 weeks. At 24 weeks her membranes ruptured and then there was foetal distress. That prompted a decision to do an emergency Caesarean section. She gave birth to a little girl weighing 575gms who survived only 42 days.
She then had two first trimester miscarriages.
This pregnancy was progressing. She went for a routine morphology ultrasound scan at almost 19 weeks pregnant. While her baby was the right size and appeared well, cervical shortening (cervix was 2.7cm long whereas is should be 3.5 to 4.5cm long) and funnelling (opening of cervix end nearest uterine cavity) was seen. This suggested cervical incompetence. Cervical incompetence is when the cervix of the uterus is weak and opens prematurely (often in the second trimester of pregnancy) and in the absence of uterine contractions.
I advised Catherine that I was worried about cervical incompetence in view of the ultrasound findings. If that was the case it meant she would deliver very prematurely, with all the adverse implications. Personally, I have not been impressed with vaginal progesterone pessary use to prevent cervical dilatation. I have always had success with a cervical suture. I suggested to Catherine that I should insert a cervical suture to keep her cervix closed and so prevent her from delivering prematurely.
I advised her that while her recollection of what had happened in her first pregnancy was not suggestive of cervical incompetence, I could not ignore the ultrasound scan findings. I did not want her to deliver her baby prematurely because of a problem that could have been prevented. In her first pregnancy, she was managed as a public patient and had been transferred from one public hospital to another public hospital because of the complications. It would be extremely unlikely to be able to get helpful obstetric history information.
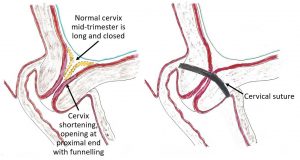 In her 19th week of pregnancy, I inserted a cervical suture. I commenced her of prophylactic low dose antibiotics, which she stayed on for the duration of the pregnancy. This was to minimise the risk of the cervical suture causing any infection problem. A tocolytic medication (drug to stop uterine contractions) was given by injections while in hospital to minimise the risk of uterine irritability with the cervical suture insertion operation. In view of the difficult history with her first pregnancy, I prescribed an oral tocolytic medication long term.
In her 19th week of pregnancy, I inserted a cervical suture. I commenced her of prophylactic low dose antibiotics, which she stayed on for the duration of the pregnancy. This was to minimise the risk of the cervical suture causing any infection problem. A tocolytic medication (drug to stop uterine contractions) was given by injections while in hospital to minimise the risk of uterine irritability with the cervical suture insertion operation. In view of the difficult history with her first pregnancy, I prescribed an oral tocolytic medication long term.
I started seeing her weekly. This was both for her own reassurance (she was becoming more nervous about the pregnancy) and, so I could monitor her more closely.
At 23 weeks Catherine did become aware of uterine irritability. This was managed with rest and adding a second oral tocolytic medication, to be taken when she had contractions. At 25 weeks pregnancy, the dose of the original oral tocolytic medication was increased because of contractions. At 29 weeks the dose of the second tocolytic medication was increased because of contractions. A steroid, Celestone Chronodose, was given in two injections 24 hours apart to minimise the likelihood and severity of immature lungs (hyaline membrane disease) if there was preterm delivery.
An ultrasound scan done by a specialist pregnancy ultrasound scan unit at 30 weeks and reported her baby was a good size (47th centile or 1414gms weight). It also reported the cervical suture was well positioned and the cervix measured 2.8cm long.
The pregnancy progressed well, though she needed to continue to rest and remained on the tocolytic medications because of uterine irritability.
We decided on delivery at 37 weeks. That was because Catherine was understandably becoming more nervous. As well I did not want her going into labour with the cervical suture in situ and with the uncertainty about the details of her previous Caesarean section. It was likely that the lower segment had not been very developed at 24 weeks, and so there was an increased risk of uterine rupture with advanced gestation and especially with labour. A further injection of Celestone Chronodose was given to minimise the likelihood of her baby having immature lungs and transient tachypnoea of the newborn after birth. We wanted it to be a ‘family friendly’ Caesarean section with her baby and her partner staying with her in theatre and recovery ward and then going to the postnatal ward as a family. We did not want her baby having to be admitted to the Special Care Baby Unit with breathing problems.
The Caesarean section delivery done at 37 weeks and 3 days gestation and was uncomplicated. She had the operation under a combined spinal-epidural anaesthetic. Her daughter Sienna had a birth weight of 2430gms. Sienna was born in excellent condition and was able to stay with her parents in the operating theatre while I completed the operation, in the recovery ward and on the postnatal ward.
Closure took a considerably longer time than usual. Bowel and omentum were adherent to the inside of the abdominal wall. These adhesions were divided carefully avoiding traumatising bowel. Then the abdominal wall was closed in all layers, which is my usual practice. I suspect this had not been done with closure at her first Caesarean section because of the considerable adhesions and the considerable midline gap of her rectus abdominis muscle. After completing the Caesarean section, the cervical suture was removed.
Mother and daughter were discharged home together with Catherine successfully breastfeeding Sienna.
Catherine and her partner are so, so happy that they have been blessed with a beautiful little girl. I am so pleased that through careful management I was able to successfully support Catherine in her pregnancy and delivery and share with her and her partner the joy of the birth of a healthy baby girl.

