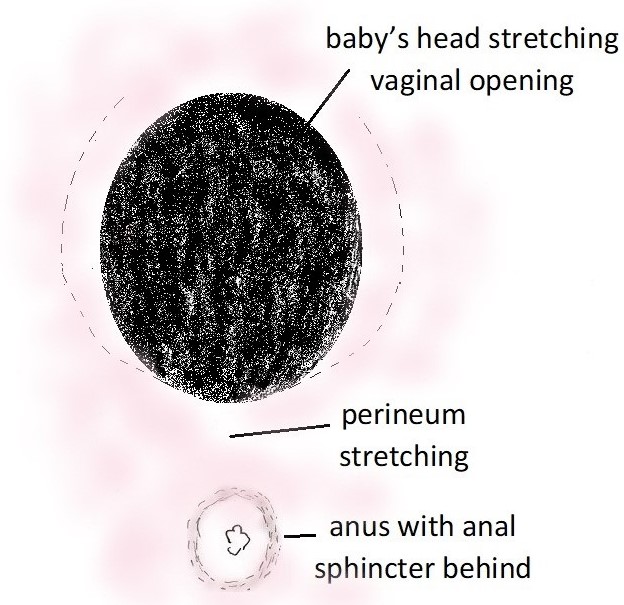
Rosemarie saw me for management of her first pregnancy. The pregnancy was uneventful. She was admitted to hospital in spontaneous labour when she was 39 weeks gestation. She had an epidural for pain relief in labour. In second stage labour there was slow progress with pushing. As well the baby’s heart rate pattern was abnormal and suggested foetal distress. Baby was in a right occipito-posterior position (viz. baby was “looking up” rather than “looking down”). I discussed the situation with Rosemarie and her husband, and it was agreed for an operative vaginal delivery. I used the MityOne vacuum. Baby’s head was delivered in the occipito-posterior (OP) position with the vacuum cup. There was no rotation of baby’s head to an occipito-anterior (OA) position. I delivered the baby’s head slowly with a combination of maternal pushing and traction on the vacuum handle. I carefully watched her perineum for any early signs of tearing. There was increased likelihood of tearing because of the occipito-posterior position of baby’s head. With an occipito-posterior position the head is deflexed and so there is a greater diameter of the head presenting. This causes greater stretching of the vaginal entrance and so a greater likelihood of tearing. There was no tearing. Rosemarie’s perineum remained intact. No perineal repair was needed. No stitching was needed. Her daughter was born in good condition and had a birth weight of 3070gms.
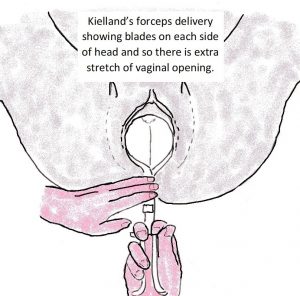 In the past vacuum devices were less reliable and would frequently come off baby’s head with traction. Because of this I used forceps to delivery baby’s head when an operative vaginal delivery was needed. As Rosemarie’s baby’s head was in an occipito-posterior position, in the past I would have rotated the baby’s head to an occipito-anterior position with Kielland’s forceps and delivered baby’s head in the occipito-anterior position. I would have rotated baby’s head because there is increased likelihood of significant perineal trauma if baby’s head is delivered in the occipito-posterior position with forceps. That is because there is greater stretching of the vaginal opening with an occipito-posterior position. This vaginal opening stretching is even more because forceps blades on each side of baby’s head. I would have done an episiotomy to reduce the increased risk of significant perineal trauma with using forceps.
In the past vacuum devices were less reliable and would frequently come off baby’s head with traction. Because of this I used forceps to delivery baby’s head when an operative vaginal delivery was needed. As Rosemarie’s baby’s head was in an occipito-posterior position, in the past I would have rotated the baby’s head to an occipito-anterior position with Kielland’s forceps and delivered baby’s head in the occipito-anterior position. I would have rotated baby’s head because there is increased likelihood of significant perineal trauma if baby’s head is delivered in the occipito-posterior position with forceps. That is because there is greater stretching of the vaginal opening with an occipito-posterior position. This vaginal opening stretching is even more because forceps blades on each side of baby’s head. I would have done an episiotomy to reduce the increased risk of significant perineal trauma with using forceps.
Perineal tears are classified according to severity of tearing:
- 1st degree: perineal skin only torn.
- 2nd degree: perineal skin, perineal muscles, but not the anal sphincter torn.
- 3rd degree: perineal skin, perineal muscles, and anal sphincter torn.
- 3rd degree tears are subdivided according to severity of anal sphincter tearing:
- 3a: less than 50% thickness of external anal sphincter.
- 3b: greater than 50% tear of external anal sphincter.
- 3c: greater than 50% tear of the external anal sphincter and internal anal sphincter.
- 4th degree: perineal skin, perineal muscles, and anal sphincter and rectal mucosa torn.
Most perineal tears are 2nd degree. Often a minor 2nd degree tear is called a 1st degree tear, by the accoucheur (person who assists the women with childbirth).
Sometimes an episiotomy extends with tearing so there can be combination of episiotomy and significant perineal tearing to repair. This risk is less with a more lateral medio-lateral episiotomy and very careful delivery of the baby’s head.
Significant perineal trauma
Significant perineal trauma is when there is a more extensive 2nd degree tear, episiotomy and tear or a 3rd or 4th degree tear. With significant perineal trauma there needs to be careful repair to restore the anatomy and to minimise the risk of ongoing problems. Concerns with significant perineal trauma include:
- Greater postnatal perineal pain.
- Wound breakdown and the need for resuturing. Sometimes the open wound is left to heal gradually.
- Ongoing perineal discomfort because of scar tissue.
- Painful sex because of scar tissue.
- Revision of scar tissue in the operating theatre under a general anaesthetic.
- If 3rd or 4th degree tear faecal incontinence and / or faecal flatulence.
- If 4th dree tear also risk of rectovaginal fistula (hole forms between rectum and vagina) developing that results in some faecal material being passed via the vagina.
Avoiding significant perineal trauma is a major consideration with a vaginal delivery.
Many years ago, a patient moved to Perth in advanced pregnancy. I next saw her when she attended for a consultation about a year after delivery. She had faecal incontinence. She said the doctor who delivered her baby had failed to recognise she had anal sphincter tearing with the delivery. Her anal sphincter was not repaired. I referred her to a colorectal surgeon, but it was too late. He could nor repair her anal sphincter. So, she now has a permanent colostomy bag. There was incredible marital strain consequently and eventually her husband left her.
There are several factors relevant in determining the likelihood of significant perineal trauma with a vaginal delivery…
• Elasticity of tissues. This is a part of a woman’s makeup and I consider the most important factor in determining whether there will be perineal trauma with delivery. Some women have a ‘stretchier’ perineum, that stretches well with the baby’s head coming through. This was the case for 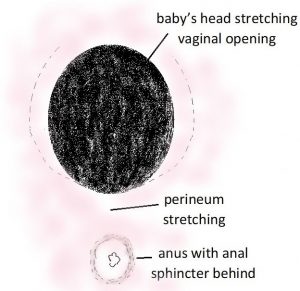 Rosemarie.
Rosemarie.
Some women can deliver a baby with a birth weight more than 4Kg without any tearing. Such women have considerable elasticity of their tissues. In contrast with some women there is superficial tearing of the perineum or vaginal tearing even before the baby’s head is crowning and when this is not excessive stretching of the lower vagina and vaginal entrance. If this happens it a very ominous sign a tasty tear will happen. It is much safer for these women to have a medio-lateral episiotomy, that safeguards the perineum.
Most women have tissue elasticity between the two, where there can be some stretching without tearing, but sometimes not enough elasticity to avoid tearing with the stretching caused by baby’s head. These women need careful management of delivery to avoid or minimise perineal trauma with delivery.
• Previous childbirth. While the vagina and vaginal opening go back to almost their normal size after a delivery, for all women there is some degree permanent stretching of the vagina and vaginal opening after a vaginal delivery. Because of this second stage is usually a lot quicker and easier for a woman in her second and subsequent vaginal births than in her first. Because of this permanent stretching of the vaginal opening, there is usually less perineal trauma with the second delivery than then first.
But if a woman had significant trauma with her first delivery that has resulted in significant scar tissue with healing this is not necessarily the case. Scar tissue does not have the same degree of elasticity as non-scarred tissue and is more likely to tear. So, significant trauma with the first vaginal delivery predisposes the woman to significant trauma with another vaginal birth. There needs to be very careful management of the delivery by an experienced accoucheur and often an episiotomy is indicated to offset the risk of tearing and avoid a repetition of her first-time trauma.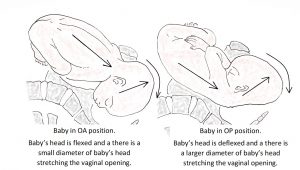
• Position of baby’s head. If baby’s head is in an occipito-posterior (OP) position the head is more deflexed than it would be if it were in an occipito-anterior (OA) position. This means with an occipito-posterior position there is greater diameter of the head presenting, greater stretching of the vaginal entrance resulting a greater likelihood of significant perineal tearing.
• Size of baby. The larger the baby the greater the likelihood of significant tearing. But sometimes with a preterm delivery of a smaller baby there can be significant perineal trauma because of the lack of elasticity of the woman’s vaginal entrance.
• Tone of pelvic floor muscles. Sometimes women who are at a high level in a sport, especially sports which can result in particularly good tone of her pelvic floor muscles (e.g. horse riding, gymnastics, body building, ballet, yoga) can find it difficult to relax their pelvic floor muscles in second stage labour. This adversely effects their chances of having a spontaneous vaginal delivery and avoiding significant perineal trauma. Sometime an epidural and sometimes and episiotomy can help.
• Control of baby’s head with delivery. If there is a slow and controlled delivery of baby’s head, there is a much greater likelihood of no perineal trauma. That is because there is slow and more gradual and controlled stretching of the vaginal entrance. This is when an epidural can help. An epidural takes away what can be an overwhelming desire of the woman to push excessively and in an uncontrolled way when the baby’s head is crowning. A couple of weeks ago a patient delivered in the ambulance on route to the hospital. These was no control of baby’s head as it delivered. She had major perineal trauma that involved the anal sphincter.
• Experience of the accoucheur. With supporting more women with vaginal deliveries comes more knowledge, wisdom and experience and 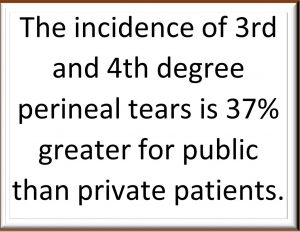 so greater likelihood of avoiding nasty perineal trauma. Furthermore, if there is significant tearing an experienced obstetrician will have greater expertise in recognising the anatomy involved and in suturing correctly and so minimising the likelihood of ongoing problem for the woman.
so greater likelihood of avoiding nasty perineal trauma. Furthermore, if there is significant tearing an experienced obstetrician will have greater expertise in recognising the anatomy involved and in suturing correctly and so minimising the likelihood of ongoing problem for the woman.
• Private or public pregnancy care. The incidence of significant perineal trauma is greater for public than private patients. The incidence of 3rd and 4th degree perineal tears is reported to be 37% greater for public than private patients(1). A private patient is managed by a fully qualified specialist obstetrician doctor. In contrast frequently public patients have spontaneous vaginal deliveries often managed by trainee (student) midwives or less experienced midwives. Typically, operative vaginal deliveries of public patients are done by trainee obstetricians (registrars and senior registrars). I have had many women see me for their second pregnancy management after a very traumatic delivery as public patient with their first.
Furthermore, if there is significant trauma repair as a private patient repair is done by fully qualified specialist obstetrician doctor (and often with the support of a colo-rectal surgeon if a 4th degree anal sphincter tear) and so there should be a good outcome. For a public patient repair is often done by a less experienced trainee obstetrician (registrars and senior registrars) and the long-term result may reflect this.
• Episiotomy. While some women are very anxious about an having episiotomy, 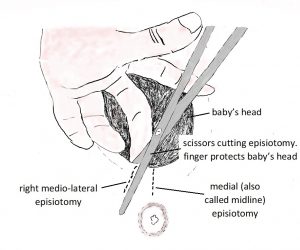 a medio-lateral episiotomy is much safer than having a nasty perineal tear.
a medio-lateral episiotomy is much safer than having a nasty perineal tear.
Often in the past (and sometimes now) episiotomies were cut in a medial direction viz in the midline in the direction of the anal sphincter. There is risk of anal sphincter involvement with such midline episiotomies by actual cutting or the episiotomy extending with tearing.
With a medio-lateral episiotomy the scissor cut in the direction of the right buttock and so the episiotomy avoids the anal sphincter and perineal muscles. With careful suturing repair of the episiotomy there is usually excellent healing. A woman will feel much more comfortable than she would after a nasty perineal tear and the risk of anal sphincter involvement is minimised.
• Forceps delivery. As mentioned forceps are positioned on either side of baby’s head and so cause greater stretching of the vaginal entrance than happens with a spontaneous vaginal delivery or with a vacuum delivery. Hence there is greater risk of significant perineal trauma if forceps are used. This risk can be offset by cutting a right mediolateral episiotomy. But even then if there is poor elasticity of tissues the episiotomy cut can extend and there can be significant tearing. The minimise this risk I do a more lateral aimed and more generous length mediolateral episiotomy when doing a forceps delivery. But my preference is a spontaneous vaginal delivery, but if an operative vaginal delivery is needed to use a vacuum cup. I do few forceps deliveries these days.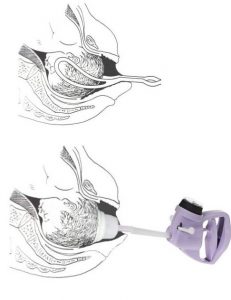
There is less risk of significant perineal trauma with a vacuum than forceps because the vacuum cup is applied by suction to the top of baby’s head and so there is no more stretching of vaginal entrance than would be the case for a spontaneous vaginal delivery. As well there is extra control of the delivery of the head so it can be done very slowly and so also help minimise the likelihood of perineal trauma.
Epi-No. The jury is still out about the value of the Epi-No. If the Epi-No was as good as the manufacturer says, then the Epi-No would now be extremely popular. But the lack of popularly suggests the Epi-No is not highly regarded in the community. Medical studies have mixed results. Some say it is of benefit, others say it is not. The women who use it and have no perineal trauma are more likely tell others how good it is, but it may be these women have intact perineums after delivery because of their tissue elasticity and so their lack of perineal trauma had nothing the do with the Epi-No. But certainly, the Epi-No will not do harm. If a woman wants to go to expense of buying an Epi-No and conscientiously using it before labour, I have no objections.
Perineal massage. This is often recommended, but the evidence that it is of any benefit is lacking. It is medically illogical to consider it will make any difference. But certainly, it will not do harm. If a woman wants to conscientiously do it before labour, I have no objections.
There are no guarantees
Despite the best care by an extremely experienced accoucheur there can be significant perineal trauma. The likelihood is less when delivery is as a private patient and managed by an experienced obstetrician.
And next time?
Some women will defer having another pregnancy because of the ‘traumatic’ childbirth they experienced. I suggest to such woman it would be better if they have a Caesarean section delivery next time. With a Caesarean section there will be no risk of further perineal trauma and they can have much more enjoyable pregnancy and childbirth experience knowing this
Many women are keen for vaginal delivery next time even though they sustained significant perineal trauma. This is a concern if there has been anal sphincter tearing. If there is repeated anal sphincter tearing with delivery there is significant risk of permanent anal sphincter weakness, faecal incontinence, and the need for a permanent colostomy.
If a woman who has had a 4th degree tear or 3rd degree tear it is much safer for her to have a Caesarean section next time. If it was only minor degree of anal sphincter tearing (3a classification) and the woman insists on a vaginal delivery then, I am prepared to support her if she agrees to it being a controlled delivery. I encourage delivery before the baby gets large, so there is increased likelihood of labour induction. I encourage an epidural, so these is more control of delivery of baby’s head and more gradual vaginal opening stretching with delivery. I encourage a right mediolateral episiotomy to minimise the likelihood of perineal tearing. I managed a patient in this way recently after a minor degree of anal sphincter tearing with her first delivery. All went to plan. She had a straightforward episiotomy with no tearing which was much more comfortable postnatally and is healing well.
One advantage of a vaginal delivery is that it can stretch the vaginal tissues and so stretch any scar tissue that may be causing ongoing discomfort.
But these needs to be careful management of the delivery in order the minimise the likelihood of further significant trauma. There should be very slow and controlled delivery of baby’s head. There is a likelihood that an episiotomy is needed because scar tissue in the perineum (formed with healing of the perineum) does not have the same elasticity and normal tissue and so is more likely to tear.
Some women who experienced significant physical trauma with a vaginal delivery also experience considerable emotional trauma because of ongoing physical issues and because their first delivery did not go according to their birth plan. Because of this they can feel ‘cheated’ and can be determined to have the vaginal delivery experience second time they consider they were denied first time. This is a huge management challenge. While an obstetrician /midwife should be sensitive to their emotional trauma and birth plan requests, the primary focus must be the patient and her baby’s physical wellbeing and minimising physical trauma this time. But such women can be reluctant to accept the need for the careful management of the delivery and that extra steps may be needed to avoid a repetition of their first childbirth experience. There needs to be careful detailed discussion of the increased risks of a vaginal delivery in her case and benefits of planned management. But if the woman declines medical advice, then she must accept responsibility for the consequences of her decision. A colleague had a patient who he encouraged to have an episiotomy, as he was very concerned she would have nasty perineal tear without an episiotomy. He advised her of the possibility of a 3rd degree tear without the episiotomy. She insisted she did not agree to having an episiotomy. She had a major 3rd degree tear. Her 3rd degree tear would most likely have been avoided if she had agreed to having an episiotomy.