Posterior Placenta Position – Placenta Praevia
It was a Thursday afternoon. I took a patient to theatre for a Caesarean section delivery because of the Posterior Placenta Position which is called placenta praevia.
Placenta praevia is when the placenta develops in the lower aspect of the uterus and in close relation to the cervix. In this case, the ultrasound scan indicated the placenta was on the anterior wall of the uterus, covered the cervix and extended onto the posterior wall to at least 5cm. As well the baby was in an oblique lie with the head being on the left side of the uterus.
The main danger of placenta praevia is excessive bleeding. Fortunately, this did not happen with this patient. There had been no bleeding except minor spotting.
The Caesarean section was done under a spinal anaesthetic. The entry through the abdominal wall went well. The bladder was deflected from the front of the uterus to avoid the risk of it being traumatised with the uterine incision. There was superficial transverse scoring of the uterine wall with the scalpel blade in the lower segment where I wanted the hole in the uterine wall to be. There were no prominent uterine vessels in the lower segment region and so there was not excessive bleeding when cutting through the uterine wall. The scalpel incision through the uterine wall was about 3cm long and was transverse midline in the lower segment of the uterine muscle, where it has been scored. I then inserted both index fingers into the hole made by the scalpel and split the uterine muscle transverse alone the line of the score mark so the hole was big enough to deliver the baby.
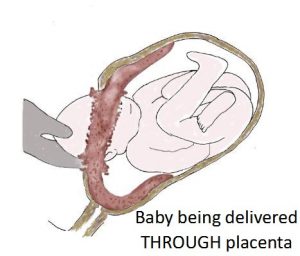 After making the hole in the uterus the placenta was seen. The placenta was immediately below the uterine wall incision and was obstructing access to the uterine cavity and to the delivery of the baby. I tried to go around the placenta with my hand to get to the baby by separating the placenta from the uterine wall. I soon realised this would mean too much placental separation before the baby was born. I decided instead to make a hole through the placenta below the middle of the uterine wall incision. The amniotic sac was then opened and clear amniotic fluid flowed out. With my hand now in the uterine cavity, I moved my hand to the left side of the uterus where the baby’s head was. I guided the baby’s head to the midline below the uterine wall hole. With my guiding hand now cupping the head of the baby and my assistant pushing on the top (fundus) of the uterus, the baby’s head started to deliver through the placenta, hole in the uterus and abdominal wall incision. I removed my hand to make more room for the head to come through the hole in the uterus wall. The rest of the head and then the body of the baby was safely delivered. There was a ring of placenta around the head as it came through the uterus wall because the delivery of the baby was through the hole I had made in the placenta.
After making the hole in the uterus the placenta was seen. The placenta was immediately below the uterine wall incision and was obstructing access to the uterine cavity and to the delivery of the baby. I tried to go around the placenta with my hand to get to the baby by separating the placenta from the uterine wall. I soon realised this would mean too much placental separation before the baby was born. I decided instead to make a hole through the placenta below the middle of the uterine wall incision. The amniotic sac was then opened and clear amniotic fluid flowed out. With my hand now in the uterine cavity, I moved my hand to the left side of the uterus where the baby’s head was. I guided the baby’s head to the midline below the uterine wall hole. With my guiding hand now cupping the head of the baby and my assistant pushing on the top (fundus) of the uterus, the baby’s head started to deliver through the placenta, hole in the uterus and abdominal wall incision. I removed my hand to make more room for the head to come through the hole in the uterus wall. The rest of the head and then the body of the baby was safely delivered. There was a ring of placenta around the head as it came through the uterus wall because the delivery of the baby was through the hole I had made in the placenta.
Once the baby was delivered the cord was quickly clamped. We had to move very quickly once incision of the uterus was made because with displacement and trauma to the placenta there was a risk of the baby losing blood. But all went well and the baby was born in good condition. The baby was a little girl weighing 3270gms. Mum’s blood loss was not excessive. There was no concern about the baby having blood loss. The placenta was delivered after the baby.
Two weeks later I had another Caesarean section planned for placenta praevia. This time it was a posterior placenta position that covered the cervix extended onto the anterior wall to about 5cm, by ultrasound scan checking.
In contrast to the first patient, this patent had episodes of significant vaginal bleeding. She required hospitalisation because of bleeding.
It was late on the Sunday evening before she booked a Caesarean section the next Thursday. I was contacted by the midwife to tell me there was about 300mls of bleeding and the onset of contractions. Labouring with placenta praevia is very dangerous. The placenta is below the baby and obstructs the birth canal. Labouring with placenta praevia will cause very excessive bleeding and so is very dangerous for mother and baby. I advised I needed to do an immediate Caesarean section. The Caesarean section delivery was done at about midnight under a spinal anaesthetic.
The entry through the abdominal wall went well. The bladder was deflected. Then I did superficial transverse scoring of the uterine wall with the scalpel blade where I wanted the hole in the uterine wall to be. This time there were prominent uterine vessels in the lower segment region, in the line where I needed to cut. This scenario is not unusual with placenta praevia as there is more blood flow to the region of the uterine wall where the placenta is attached. The cutting of these large blood vessels resulted in excessive uterine wall bleeding. There was too much blood pooling to see the uterine muscle I was cutting. This meant I could not see when I had cut through the full thickness of the uterine wall. Baby’s head was only millimetres below the uterine wall incision. I didn’t want to risk cutting too deep and accidentally cutting baby with the scalpel. So, I decided to tunnel through the uterine wall with my index finger. A hole made by my finger rather than a scalpel blade was a much safer option. Once through the uterine wall, I proceeded to split the uterine wall using my two index fingers transverse in the lower segment along the scoreline.
This time it was easy to get around the placenta as it was mostly the posterior placenta position and then to deliver the baby. Once the baby was delivered the cord was quickly clamped. We had to move very quickly once incision the uterus as with displacement and trauma to the placenta as there was a risk of the baby losing blood. The baby was born in good condition. The baby was a little girl weighing 3010gms. Extra suturing and diathermy were needed to stop the cut vessels in the uterine wall bleeding. Haemostasis was achieved, though blood loss was more than usual.
Posterior Placenta Position – Placenta praevia is one of the most dangerous complications of pregnancy
Placenta praevia is one of the most dangerous complications of pregnancy and it can be associated with very heavy bleeding. Placenta praevia bleeding is described as ‘painless, purposeless and profuse’ (the 3Ps of placenta praevia). Painless means it can happen without any discomfort. Purposeless means the bleeding can happen without warning or activity (though activity should be limited when there is placenta praevia and there should be no sexual intercourse). Profuse means the bleeding can be very excessive. Women describe how they wake from their sleep thinking they have wet the bed only to find the bed sheets are covered in blood.
These days (in contrast to the past) it does not automatically mean hospitalisation. Hospitalisation is needed if there is significant bleeding. If only minor bleeding there needs to be immediate attendance at the Birth Unit to be checked, no matter what the time of day. In the past, a woman with placenta praevia was kept in hospital for weeks until delivery and blood was kept cross-matched in case an urgent blood transfusion was needed.
The blood loss is from the mother and not from the baby. Baby’s wellbeing is ok, as long as blood loss is not so excessive that it is a risk to maternal well-being. With placenta praevia mother will suffer before baby. In other words, if mum is ok then the baby is ok.
In all cases except minor (called grade 1) placenta praevia delivery is by Caesarean section. That is because when the placenta is below the baby it would deliver before the baby with a vaginal delivery. There would be life-threatening bleeding for the mother and considerable risk to the baby due to lack of oxygen and blood loss with premature placental separation with a vaginal delivery. Caesarean section for placenta praevia is potentially one of the most dangerous and difficult Caesarean sections and ideally should only be done by an experienced obstetrician. Mind you that does not always happen. My first solo (unsupervised) Caesarean section was for anterior placenta praevia. It was many years ago when I was a very junior registrar. The senior registrar said to me he was going to be about 30 minutes away in another hospital if I needed him (Hmmm…). All I had was the assistance of a junior resident doctor. The women did not know about my lack of experience. Fortunately, all went well.
In the past, a placenta praevia Caesarean section was always under a general anaesthetic and the operation was not started until there were four units of cross-matched blood in the operating theatre in case an urgent blood transfusion was needed.
Incidence and risk factors of Posterior Placenta Position – Placenta Praevia
Placenta praevia occurs in about 0.5% of all pregnancies. The incidence is reported to increase 1.5 to 5-fold with a history of previous Caesarean section delivery. I have done thousands of Caesarean sections and this has not been my experience. I suspect it is because I am very careful to avoid suturing the inner uterine wall non-muscle layer (endometrium, called decidua in pregnancy) and so embedding endometrium tissue in the uterine muscle with uterine wall closure.
When there is an anterior placenta praevia under a previous Caesarean scar there is increased risk of placenta accreta, where the placenta is embedded in the uterine wall and cannot be easily separated from the uterine wall at delivery. This is an extremely dangerous and life-threatening complication for the mother. Personally, I have never had a situation where the placenta was so adherent that I could not remove from the uterine wall after delivering the baby. Again, I suspect it is because I am very careful to avoid suturing the inner uterine non-muscle layer (endometrium, called decidua in pregnancy) and so embedding endometrium tissue in the uterine muscle with uterine wall closure.
There is also increased risk of placenta praevia with a history of other uterine surgery such as myomectomy (removal of fibroid), previous uterine rupture or perforation, excessive curettage with a dilatation and curettage of uterus procedure (especially if after a failed pregnancy)
Advanced maternal age increases the incidence of placenta praevia. After age 35 years the incidence is reported to be 2% and after age 40 years to be 5%.
Low lying placenta at the 19-week morphology scan
A low-lying placenta is often mentioned at the 19-week morphology scan. This does not mean the woman will need a Caesarean section delivery for placenta praevia. While the placenta does not move its relation to the cervix can change as the uterus wall enlarges as the pregnancy advances.

