“I have itchy hands and itchy feet”
This pregnancy progressed well until her routine antenatal visit at 35 weeks 0 days when her baby measured smaller than dates. I estimated baby’s weight to be 2473gms. I sent her for foetal growth and wellbeing scan which reported her baby’s wellbeing was good and that her baby had an estimated weight of 2442gms, which was on the 22nd centile for 35 weeks.
 Labour was induced the next day when she was 35 weeks and 5 days gestation. She laboured well, with the total duration being 2 hours. She went on to have normal vaginal delivery of a healthy baby boy weighing 2545gms.
Labour was induced the next day when she was 35 weeks and 5 days gestation. She laboured well, with the total duration being 2 hours. She went on to have normal vaginal delivery of a healthy baby boy weighing 2545gms.
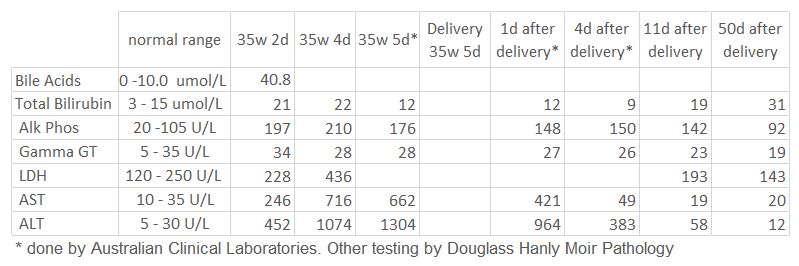
Both mother and baby have done well. It had taken a while for Bronwyn liver enzymes to return to normal. Bronwyn’s bilirubin is mildly elevated at the last check on 25th Sept 2017 at 31umol/L. Her bilirubin had been 34 umol/L in April 2016 with normal liver enzymes. The most likely reason for her mildly elevated bilirubin is she coincidentally has a benign liver condition called Gilbert’s syndrome. I could not find any evidence in the medical literature that Gilbert’s syndrome is relevant in the aetiology of obstetric cholestasis.
Obstetric cholestasis is also called intrahepatic cholestasis of pregnancy, cholestasis of pregnancy and cholestatic jaundice of pregnancy. Obstetric cholestasis is the most common liver disorder in pregnancy and occurs in about 1% of pregnancies. It is caused by a reduced excretion of bile salts by the liver, which leads to increased serum bile acids. These bile salts are deposited within the skin, causing pruritus or itchy hands and feet in pregnancy.
The cause of obstetric cholestasis is unknown but is thought to be multifactorial with hormonal, genetic and environmental possible factors. Oestrogen has a known role in causing cholestasis. Hence it happens in pregnancy, but as well it can happen when taking an oestrogen-containing contraceptive pill. It is also as associated with progesterone use in pregnancy, to prevent preterm delivery. There is also a genetic component to the aetiology as it is more common when there is family history of obstetric cholestasis or cholestasis with oral contraceptive use. As well, it is more common in women of South Asia, South America, and the Scandinavian countries. It is more common in winter, with advanced age, with multiparity and with twin pregnancies.
Obstetric cholestasis recurs in 45-70% of subsequent pregnancies. Whether this high incidence of recurrence is due genetic factors or due to background health issues is unknown. When it does recur, it is usually less severe.
It most often presents in the late second or early third trimester of pregnancy. It is characterized by pruritus that begins in the periphery of the body, often worse on the palms and soles, and which moves centrally to the trunk and face with no other skin manifestations. The pruritus can become very intense and persists and worsens as pregnancy continues. Bronwyn’s itch was not severe. It usually resolves within 48 hours of delivery. The pruritus is often worse at night and may be so severe that it causes sleep disturbance, irritability, and psychiatric disturbances. Up to 25% of patients develop jaundice, usually 1-4 weeks after the onset of pruritus. Bronwyn did not have jaundice. While there is no rash some patients, have excoriations caused by scratching. Some patients may develop constitutional symptoms chills and abdominal pain, and diarrhoea.
Maternal outcome is good, with symptoms resolving after delivery. There is a small risk of persistence and long-term liver disease including chronic hepatitis, liver fibrosis/cirrhosis, hepatitis C, gallstones, cholecystitis, and nonalcoholic pancreatitis.
Obstetric cholestasis is associated with spontaneous preterm labour (30-40%), meconium-stained liquor (up to 45%), and increased perinatal morbidity (usually due to preterm birth) and mortality. Without active management of pregnancy there is a 10-15% perinatal mortality rate. With active management the current perinatal mortality rate is less and is reported to be up to 3.5%. Rates of stillbirth increase after 37 weeks gestation, thus supporting active management of delivery at 37 weeks, but there have been case reports of fetal death from 31 weeks.
The medical treatment of choice is a medication called ursodeoxycholic acid. Use of ursodeoxycholic acid can help reduce the pregnant woman’s itch and can make it safer to continue the pregnancy, which is especially important if obstetric cholestasis occurs at an early gestation. Topical treatments are unlikely to be successful for the treatment of pruritus caused by cholestasis.
The cause for stillbirth with obstetric cholestasis is still unknown. Foetal mortality does not seem to be due to chronic placental insufficiency and it is not associated with intrauterine foetal growth retardation. It is thought due to an acute hypoxic event, but why this happens is unknown. There needs to be close monitoring of baby once the diagnosis is made until delivery, though this is of limited value as there have been reported stillbirths within hours of a normal cardiotocogram (foetal heart rate) recording.
Because the incidence of stillbirth increases with advancing gestation and is uncommon before 36 weeks, delivery is usually done at 37 weeks. This gestation is associated with a low risk of both stillbirth and prematurity issues. As well, failed induction of labour is less likely than it would be at an earlier gestation. Some women have such intense itching that they are extremely keen for delivery before 37 weeks. I delivered Bronwyn’s baby at 35 weeks and 5 days gestation because of the marked deterioration in her liver function.
If you have any concerns about itchy hands and feet in pregnancy or to find out more information, get in touch with Dr Sykes today.

