 This is a topic of conversation early in every pregnancy. It is important to consider this and work out what you want to do.
This is a topic of conversation early in every pregnancy. It is important to consider this and work out what you want to do.
There are three ‘screening’ options available:
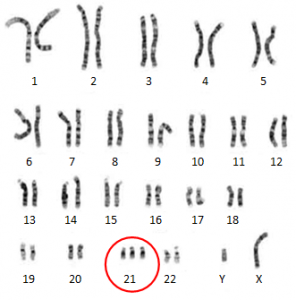
1. No checking. Many patients opt for this as they would not do anything with an abnormal result. A karyotype abnormality (as with Down syndrome) cannot be corrected. So there is only one thing that can be done, if someone wants to be proactive with the result. If a couple tell me they would not consider termination of pregnancy even if they knew the baby had Down syndrome then I recommend no testing. Why potentially subject your baby to the risk of miscarriage (as is the potential with the NTS screening with an abnormal result) and why pay extra money (more so with the NIPT) if you would not act on an abnormal result? Some say: “It will prepare me”. My experience is an abnormal result causes more worrying. I have patients who have had abnormal NTS and serum result but did not have an amniocentesis because of the risk of miscarriage. They are more stressed than if they had not had the NTS test. As well, Down syndrome has a spectrum of severity and a variety of other associated health conditions. ‘Knowing’ does not prepare you for the outcome in your baby’s case and usually people tend to conclude their baby will be the worse case and so can be very stressed.
2. The nuchal translucency scan (NTS) with serum. This is reported at about 92% accurate (and so will miss 8% of Down syndrome). As well, one in 20 will be reported as abnormal. A patient with a ‘high risk’ result usually wants further testing. This can be done through option 3 below, the non-invasive prenatal testing (NIPT), or by amniocentesis or chorionic villus sampling (CVS). An amniocentesis or chorionic villus sampling has a one in 200 to one in 300 risk of miscarriage. So it is possible for a pregnant woman to have an NTS with serum to ‘reassure her’, the result comes back as ‘high risk’, so she has an amniocentesis to ‘reassure her’, she miscarries as a direct consequence of the amniocentesis and is then told the amniocentesis result said her baby’s chromosomes are normal and there is no Down syndrome. This is uncommon, but I have had to support patients through this tragedy – knowing if the NTS test had not had done they would be cuddling their babies.
3. Non-invasive prenatal testing (NIPT). This is relatively new and many people and GPs have not heard of it. From 10 weeks, there is usually enough of your baby’s DNA in your blood to make it possible for your baby’s DNA to be filtered out from a collected blood specimen and checked to see if it is normal. This screening test is much more accurate than an NTS with serum. A negative results is considered less than one in 10,000 risk of Down syndrome. As well, it is very unlikely to give you a false positive result and so the likelihood of an unnecessary amniocentesis is very low. There are cases where there is no result. In this case, a redraw of your blood is recommended. There is no Medicare rebate on NIPT testing.
| NTS + serum | NIPT | |
| When done | 11.5 – 13 weeks pregnancy | From 10 weeks pregnancy on |
| Accuracy for Down screening | Negative result means less than 8 in 100 risk | Negative result means less than 1 in 10,000 risk |
| False positive result | 1 in 20 | very unlikely |
| No result | nil | < 5% |
| Result | Immediately if serum collection days before NTS | 5 to 12 working days |
| Cost | Medicare + gap (varies.Often about $200).If high risk result and NIPT or amniocentesis needed then extra cost | Harmony test with DHM Pathology $425 |
| Patient qualifications | nil | nil |
| Checking for T21, T13, T18 | yes | yes |
| Checking for sex chromosome disorders | no | yes |
| Finding out sex of baby | no | yes |
| Checking for other chromosomes disorders | no | not with accuracy |
I tell a patient I will support her decision whatever she makes.

