Epidural and spinal anaesthetics
Contents
Who administers the spinal and epidural anaesthetics?
How are regional spinal or epidural anaesthetics given?
What are the benefits of regional epidural anaesthetics?
What are the risks of regional anaesthesia?
Does the placement of the regional anaesthetic hurt?
When can I have an epidural for labour pain relief?
How can my epidural affect labour?
How can an epidural affect my baby?
How will I feel after the placement of an epidural or spinal anaesthetic?
Will I be able to push?
When is an epidural or spinal anaesthetic contraindicated or not possible?
I am often asked questions about epidural and spinal anaesthetics. I have compiled the information below with these questions in mind.
An epidural anaesthetic is a regional (not general) anaesthetic whether local anaesthetic medication is injected into the epidural space. This is usually done through a fine plastic tube (catheter) introduced into the epidural space via an epidural needle.
The epidural space is an area that contains fatty tissue, lymphatics, blood vessels and is transversed by spinal nerve roots. It is the bony spinal canal but just outside the dura mater (‘dura’) membrane. The epidural needle is inserted via a suitable intervertebral space (space between each pair of vertebrae in the spine) into the epidural space.
A spinal anaesthetic is a regional anaesthetic where local anaesthetic medication is injected into the subarachnoid space of the spinal cord, through a fine needle.
The subarachnoid space is deeper than the epidural space. The needle is inserted into a suitable intervertebral space into the epidural space then through the dura and another membrane on the inner side of the dura called the arachnoid mater (‘arachnoid’). The cerebrospinal fluid (CSF) that surrounds the spinal cord is contained by the arachnoid mater. With a spinal anaesthetic, the anaesthetic fluid is injected into the CSF that bathes the spinal cord.
Labour pain relief
This is popularly by an epidural block. About 60% of woman request epidural anaesthetics for pain relief in labour.
Epidural anaesthetics rather than a spinal anaesthetic is used because the epidural catheter can remain in place with its open end in the epidural space usually for the duration of labour. There can be ongoing administration of local anaesthetic via the catheter and so there can be a pain-free labour and childbirth, irrespective of how long the labour lasts.
With a spinal anaesthetic, local anaesthetic medication is injected into the subarachnoid space through a fine needle, which is removed after the injection. A spinal anaesthetic only lasts until the anaesthetic wears off, which is usually after about two hours.
A spinal anaesthetic is not suitable for labour pain relief unless it is known there will be delivery within the next hour or so after the injection. It can be done for a potentially more challenging operative vaginal delivery or for a manual removal of placenta when there has not been an epidural in labour.
Sometimes a combined spinal-epidural is used. This is because the spinal anaesthetic is of faster onset (within a few minutes) and so gives quick onset and very effective pain relief. The epidural anaesthetic catheter is sited so local anaesthetic can be administered via this route so there can be ongoing pain relief in labour after the spinal anaesthetic medication has worn off.
Caesarean section deliveries
Spinal anaesthetics have become far more popular than epidural anaesthetics for elective Caesarean section deliveries. This is because spinal anaesthetics are quicker in onset and give more predictably effective pain relief. The limited duration of anaesthetic is usually not a problem as the operation is usually completed before the anaesthetic has worn off.
Sometimes a combined spinal-epidural anaesthetic is done. That gives all the benefits of the spinal anaesthetic and the epidural catheter is in place for postoperative pain relief and in case the operation takes a longer time than the spinal anaesthetic is effective.
Epidural anaesthetics are used if it is an emergency Caesarean section in labouring woman who has epidural is for pain relief in labour.
In the past epidurals were routine for elective Caesarean section deliveries as the spinal anaesthetic needles available were larger and of a different shape to those used today. Consequently, in the past, there was a relatively high incidence of spinal anaesthesia headaches (called a ‘spinal headache’) after delivery. That happens because the CSF continues to leak out through the puncture hole in the dura after the spinal anaesthetic needle has been removed. This is very uncommon with the needles used today.
I recall the days in the past when epidural anaesthetics were routine for elective Caesarean section deliveries. They took a much longer time than spinal anaesthetics to site, to be effective and sometimes despite correct location of the epidural catheter and despite waiting a long time (sometimes a longer time than was needed to do the Caesarean section) the epidural block was still not effective enough for the Caesarean section operation and so a general anaesthetic was resorted to.
Who administers the spinal and epidural anaesthetics?
A doctor who has done extra training and is qualified as a specialist anaesthetist doctor will administer the regional anaesthetic.
If is an epidural anaesthetic for labour pain relief then it will be the anaesthetist who is ‘on call’ for the Birth Unit when you are in labour. The doctor will vary from one day to the next according to the on-call roster. The midwife looking after you will contact this anaesthetist.
If you are having an elective Caesarean section on one of my regular operating lists, then it will be the anaesthetist I work with regularly who will administer your anaesthetic.
If it is an emergency Caesarean section, then it will be the anaesthetist on call or who is available at the time you need the Caesarean section.
Effectiveness
A spinal anaesthetic is more predictable effective in giving good pain relief than epidural anaesthetics. That is because the anaesthetic fluid is injected into the space where the CSF is and so spreads quicks and evenly around the nerves.
With an epidural block, the anaesthetic fluid is injected into the epidural space where there is fatty tissue. The spread of anaesthetic fluid is slower and less predictable.
Sometimes the epidural block anaesthesia is ‘patchy’ and there is still pain in some areas despite the catheter tip being in the epidural space and the procedure having been done correctly. It is due to the uneven spread of anaesthetic fluid in the epidural space fatty tissue. A patchy epidural is not due to poor anaesthetist technique. This pain can remain despite more anaesthetic being administered and even despite redoing the epidural and relocating the catheter to a difference intervertebral space. This situation is very challenging for the labouring woman as it means she has pain in labour.
How are regional spinal or epidural anaesthetics given?
Intravenous fluids will be started before the anaesthetic is administered. Sometimes spinal or epidural anaesthetics can cause a temporary fall in your blood pressure which can make you feel faint and adversely affect baby’s wellbeing for a short period. Intravenous fluids before administration will help to prevent this from happening.
Some anaesthetists prefer you sitting up and others prefer you lying on your side for the administration procedure. You will be asked to arch your back out to open the spaces between the vertebral bones of the spine and so give better access to where the epidural or spinal needle needs to go. You will need to remain very still in this position during the procedure. This position is vital for preventing problems and increasing the regional block’s success and effectiveness.
The anaesthetist will work out where to insert the needle by feeling the spines of the vertebral bones. There will also be checking for you having curvature of the spine, as this will need to be taken into consideration with the procedure. If you are morbidly obese sometimes excess fat in your back over your spine can prevent the vertebral bones being felt. If this is the case other measures such as ultrasound will be needed you identify the intervertebral spaces.
An antiseptic solution will be used to clean the skin of the lumbar back to minimise the chance of infection. The anaesthetist will inject a local anaesthetic to numb the skin where the epidural/spinal needle needs to be introduced. The epidural/spinal needle is then inserted into the numbed area between the vertebral bones.
For an epidural, a fine catheter is threaded through the needle into the epidural space. The needle is then carefully removed, leaving the catheter in place so medication can be administered either through periodic injections or by continuous infusion. The catheter is taped to the back to prevent it from slipping out.
For a spinal anaesthetic, the needle tip is introduced to the subarachnoid space where the CSF fluid it. The anaesthetist knows he/she has the right spot as a small amount of CSF runs out the needle. Once the spinal space is confirmed anaesthetist medication is injected and then the needle is withdrawn.
Which anaesthetise medication/combination of medications is used and the dosage used will vary according to the anaesthetist’s personal preferences and what is considered more appropriate for you.
What are the benefits of regional epidural anaesthetics?
An epidural block takes away the pain of labour. An epidural can help you deal with exhaustion, irritability, and fatigue experienced in labour. An epidural can help you to rest, relax more, and give you the strength you will need to deliver your baby.
By eliminating/reducing the discomfort of childbirth, most women have a more positive birth experience.
An epidural is particularly useful if it is likely you will have a more prolonged labour.
Sometimes by taking away the pain, you can have quicker and more efficient labour.
If there is uterine hypotonicity (uterine contractions are not strong enough) and Syntocinon augmentation is needed to make labour more efficient (called ‘augmentation of labour’) then this can be done without you experiencing the associated increase in pain that would be the case otherwise.
Some women have vaginismus. The necessary vaginal examinations done to assess progress in labour will not cause discomfort if there is an epidural.
If you need an operative vaginal delivery or manual removal of placenta or other vaginal procedures then these can be done without causing discomfort.
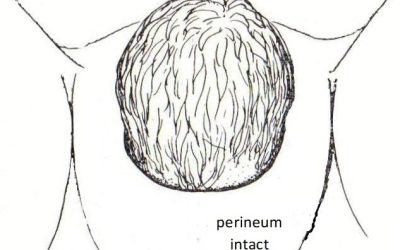
In my experience there is usually less perineal trauma in patients with an epidural as the delivery of the baby’s head can be more controlled to allow a more gradual stretch of the perineum.
If your delivery is by Caesarean section a regional anaesthetist is safer for you and your baby than a general anaesthetic. As well as you stay awake you can see your baby as it is born and enjoy your baby immediately after birth. An epidural can be used for post-Caesarean section pain relief.
What are the risks of regional anaesthesia?
Epidural and spinal anaesthetics may cause blood pressure to drop (called ‘hypotension’). This can result in you feeling faint or even going unconscious unless addressed. Hypotension can also be associated with nausea. If you become hypotensive baby’s heart rate can slow. Significant and especially prolonged hypotension is dangerous for the baby. For this reason, intravenous fluid loading is usually done before the epidural or spinal block is done. Your blood pressure will be routinely checked after you have had your regional anaesthetic. If there is a drop in blood pressure, you may need to be treated with intravenous fluids, medications, and oxygen.
You may experience a severe headache (called a ‘spinal headache’) caused by leakage of CSF. A spinal headache is associated with a spinal anaesthetic or as a complication of an epidural anaesthetic where there was unintentional piercing of the dura layer. Less than 1% of women who have regional anaesthetics experience this side effect. A spinal headache is treated with medication and if it persists with a procedure called a “blood patch”, which is an injection of your blood into the epidural space.
In rare instances (<1 in 200,000), permanent nerve damage may result from a regional anaesthetic. I have personally managed many thousands of who over many years how have had regional anaesthetics and I have never had a patient who has had this problem. This is usually raised as the reason a woman is scared to have an epidural in labour. As the incidence is so low this reason not to have an epidural should not impact a decision about pain relief in labour.
Rarely there can be an infection, bleeding around the injection site and blood vessel injury.
There is a greater risk of some complications in women who are morbidly obese as the bony landmarks used to correctly introduce the needle may not be palpable because of excess fat in the back. Refer to my website article: ‘Overweight and pregnant’.
Does the placement of the regional anaesthetic hurt?
Sometimes there is some discomfort in the area where the back was numbed, and a feeling of pressure as the small tube or catheter was placed. It is usually a very anxious patient who says she finds the procedure painful, with the discomfort related more to her fear.
Often a woman finds it is uncomfortable being curved forward to arch her back out and so to open the spaces between the vertebral bones of the spine while the epidural/spinal anaesthetic procedure is being done. There is no way around this as this position as it is necessary to give optimal access to where the epidural or spinal needle needs to go. You will need to remain very still in this position during the procedure. Once it is done you can straighten your back. This position is vital for preventing problems and increasing the regional block’s success and effectiveness. Usually, the more you can arch your back out the quicker it is to site the regional block.
When can I have an epidural for labour pain relief?
Usually, it is when you request it. This is on the conditions that you are in established labour when you make the request but, on the other hand, delivery should not be imminent.
The reason an epidural is not done before labour is established is sometimes an irritable uterus’s contractions will settle and labour does not eventuate. If you have an epidural in place and this happens you will need to have your labour induced.
Some women make their request for an epidural in very advanced labour when it is apparent that delivery is imminent. In this situation, it is likely that by the time the anaesthetic has enough time to attend and insert the epidural and it starts working you will have delivered. No anaesthetist wants to be called in and arrive after you have delivered. If it is the case that delivery is imminent the midwife will tell you accordingly. You can have nitrous oxide gas or an injection of pethidine or morphine instead.
Some women request an epidural prior to induction of labour because they want a pain free labour and delivery. It is ok to do that. Please advise me if that is your preference at an antenatal visit so I can discuss.
Sometimes a morbidly obese woman will have an epidural very early in labour or with induction if this is when the best-qualified anaesthetist is available.
Occasionally it will be recommended you have an epidural. This is usually in the context that it is apparent you are only in very early labour are not coping or it is apparent you are likely to have a long duration labour. As well it maybe you are in established labour with are coping with the contractions, but the contractions are not of sufficient strength to result in progress in labour. Syntocinon augmentation of labour is needed and it is apparent you will not cope with the extra pain that will result from stronger contractions.
How can my epidural affect labour?
This topic is covered in a separate blog article: ‘Do Epidurals Prolong Labour?’
An epidural block should not prolong first stage labour and will sometimes help reduce its duration. An epidural block will often prolong second stage labour but with careful management that usually does not mean the need for an operative vaginal delivery.
How can an epidural affect my baby?
There is no reason why your baby will be adversely affected by you having an epidural block. This comment is made with the consideration of you not having significant hypotension in labour because of the epidural. Being significantly hypotensive can affect your baby until the hypotension is corrected.
How will I feel after the placement of an epidural or spinal anaesthetic?
A spinal anaesthetic starts to work within one to five minutes. An epidural anaesthetic will take longer. You should begin to numb within a few minutes after the initial dose. You will probably feel the full benefit effect after 10 to 20 minutes
Initially, you may feel a degree of warmth in your legs followed by pins and needles in one or both of your legs. You will be asked to lie flat with a tilt as the anaesthetic block continues to work. You will experience the loss of these sensations your legs will be numb to touch and then you will be unable to move your legs. You should feel no pain below the waistline at this stage, but you may still have the sensation of pressure.
With a spinal anaesthetic, you are confined to bed/operating table as you lose all sensation in your legs. Depending on the type of epidural and dosage administered, you can be confined to your bed and not allowed to get up and move around.
The loss of sensation results in an inability to void a urinary catheter is inserted routinely with a regional block and is left in place until the regional anaesthetic has worn off or until the next day if having a Caesarean section.
You might experience with regional anaesthetic nausea, shivering, a ringing of the ears, backache, itching (due to the anaesthetic drug), headache, soreness where the needle is inserted, occasional bruising where needle inserted. Medication can be used to treat significant nausea, headache, and itching.
If you have an epidural in labour then for a few hours after childbirth the lower half of your body may feel numb. This numbness will need you to walk with assistance for a short time.
Will I be able to push?
You might find that your epidural makes pushing in second stage labour more difficult as being anaesthetised takes away the urge to push. It also makes it hard to know the direction to push. There needs to be careful management of the second stage and coaching about pushing to optimise your chances of having a spontaneous vaginal delivery. This topic is discussed in my website article: ‘Do Epidurals Prolong Labour?’
Does an epidural always work?
For the most part, epidurals are effective in relieving pain during labour. Some women complain of being able to feel pain, or they feel that the drug worked better on one side of the body. A patchy epidural is due to the uneven spread of the anaesthetic fluid in the epidural space. This is due to your anatomy and is not necessarily overcome by resisting the epidural or giving you a higher anaesthetic dose.
When is an epidural or spinal anaesthetic contraindicated or not possible?
- You are on blood thinners such as Clexane or aspirin when the regional block is considered.
- You have a low platelet count. Most anaesthetists will not do a regional anaesthetic if your platelet count is <100,000 per microliter of blood.
- You are haemorrhaging significantly or in shock.
- You need a very urgent emergency Caesarean section and there is not enough time to site a regional anaesthetic.
- You are having an emergency Caesareans section for a suspected uterine rupture.
- You are morbidly obese and the anaesthetist available does not have the skills to site a regional anaesthetic.
- You have had significant back surgery or have a back deformity that precludes a regional block.
- Have an infection on or in your back.
- Have a blood infection.
- Delivery is imminent.
- You are not in established labour.
Recent Posts
Foetal distress in first stage labour, Caesarean section avoided
Emily was in labour for her...
Vacuum cup and forceps
When are vacuum cups and...
“No idea about labour”
A midwife said to me...
Avoiding stitches with a vaginal delivery
A patient asked me this...