The Mirena intrauterine contraceptive device (IUCD) is very popular method of contraception, including for postnatal women who are breast feeding. It is good ‘spacer’ between pregnancies and good for long term contraception when the family is complete.
contraception when the family is complete.
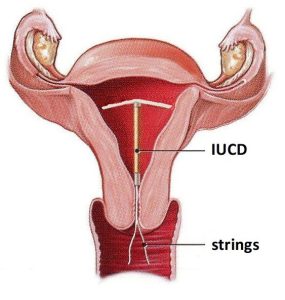
Mirena consists of a small T- shaped frame made from a plastic called polyethylene. On the stem is 52 mg of levonorgestrel, a hormone used in many contraceptive pills. There is smaller version of the Mirena called a Kyleena IUCD. It has 19.5 mg of levonorgestrel on the stem.
Benefits
- Very effective contraceptive. I have inserted hundreds and I have not had an intrauterine pregnancy yet. I’ve had one ectopic pregnancy, so it doesn’t protect against ectopic pregnancies.
- No periods or minimal periods usually.
- Can be used while breast feeding.
- Once in place a woman can forget about contraception. In contrast, if she is on the oral contraceptive pill she must remember to take it every day, if condoms they can be nuisance especially for long term use if the family is complete and are associated with a significant failure rate, if cycle timing methods they detract for the spontaneity of sexual intercourse and have a significant failure rate.
- No or minimal menstrual pain.
- Reduced adenomyosis (endometriosis in the muscle of the uterus).
- Gives permanent contraception but also a woman can change her mind. The Mirena IUCD has largely replaced sterilisation procedures for long term contraception as is as effective, safe, cheap, and results in no or minimal periods. As well, if a woman who today decides her family is complete but down the track changes her mind and wants another baby, the Mirena can simply be removed and she can conceive, whereas if there has been a female sterilisation she will need an IVF procedure and if a male sterilisation it is likely her husband / partner will no longer be producing sperm.
- Easy to insert. A Mirena IUCD inserted into a woman’s uterine cavity through her cervix. This is procedure is usually done while the woman is on the couch of an obstetrician gynaecologist examination room or in a hospital outpatient clinic. While being uncomfortable, it is not usually considered painful. The insertion procedure a bit like having a pap smear taken, though a bit more uncomfortable. There is minor bleeding usually that day only. It is effective immediately after insertion. Occasionally a woman needs to have it inserted in the hospital operating theatre under a general anaesthetic.
- Can be removed at any time, followed by a quick return to fertility.
- Reduces the risk of pelvic infection
- Reduces the risk of endometrial cancer and endometrial hyperplasia (precancer endometrial changes)
Side effects and risks
- Uterine perforation with insertion. This is rare. I have never perforated a uterus with insertion.
- IUCD partly imbedded in uterine muscle with insertion. This is not usually recognised at the time of insertion, but on a subsequent ultrasound scan. A scan would be done because of ongoing heavy periods.
- Occasionally a woman reports emotional side effects. If that is the case and the woman wants the IUCD removed, it’s very easy to do so.
- Occasionally the IUCD can slip so it is partly in the cervical canal and even protruding for the cervix. You can do self-internal check from time to time and if concerned see your gynaecologist.
- Falls out. Rarely this can happen. Check your underwear
Contraindications to having a Mirena IUCD
- Pregnant or suspected pregnant
- Have or have had pelvic infection called pelvic inflammatory disease (PID)
- Have abnormal bleeding (until reason found)
- Suspected cancer of cervix or uterus.
- Have large or abnormal shaped uterine cavity
- Allergic to levonorgestrel, silicone, polyethylene, silica, barium sulphate or iron oxide
Removal
To remove the Mirena IUCD is easy and usually painless. After introducing a vaginal speculum to visualise the cervix and strings of the IUCD, the gynaecologist pulls on the strings with a special (Rampley) forceps and out the Mirena comes through the cervix. Occasionally it can be stuck and so needs a bit more tugging. Occasionally the strings end up inside the uterine cavity and so a general anaesthetic is needed to remove the Mirena IUCD.
Mechanism of action of the Mirena IUCD
While having an inert (no progesterone) IUCD is an effective method of contraception that was popular in the past, the adding of progesterone to the stem make the Mirena an extremely effective method of contraception. The progesterone hormone is gradually released.
The progesterone causes uterine lining (endometrium) to be thin (atrophic). It is too thin for a fertilised egg to implant. As well, the progesterone will alter the cervical mucous, so the sperm can’t penetrate and in about 20% of women it will stop ovulation. But for most women, ovulation still takes place.
When should it be replaced?
- Another pregnancy. For most women it is possible to conceive immediately it is removed. If there has been suppression of ovary function a woman will have to wait until this returns.
- 5 years. The effectively in preventing pregnancy is less after 5 years and so it should be replaced then.
- If a woman has a Mirena for management of heavy periods and she or her husband / partner has had a sterilisation procedure then it can remain in place longer than 5 years and for as long as it is effective
- Can be removed after the menopause. Some women don’t know when this is as they have no periods because of the Mirena and no symptoms of the menopause. Such women should have sex hormone profile checking to establish if levels indicate a postmenopausal state.
Cost
The government very heavily subsidises the Mirena IUCD, so rather than costing about $250, it will cost about $50. It costs about $50 for five years of contraception. Plus there is the added saving of the cost of tampons and pads.

