What is a miscarriage?
Miscarriage which is also called spontaneous abortion is defined as the loss of a pregnancy before 20 weeks of gestation.
In the first third of pregnancy, a miscarriage is called a first-trimester miscarriage. A miscarriage that occurs in the second third of pregnancy up to 20 completed weeks is called a second-trimester miscarriage.
After 20 completed weeks in Australia a baby is considered to be legally viable and so a woman does not miscarry but rather experiences a preterm delivery.
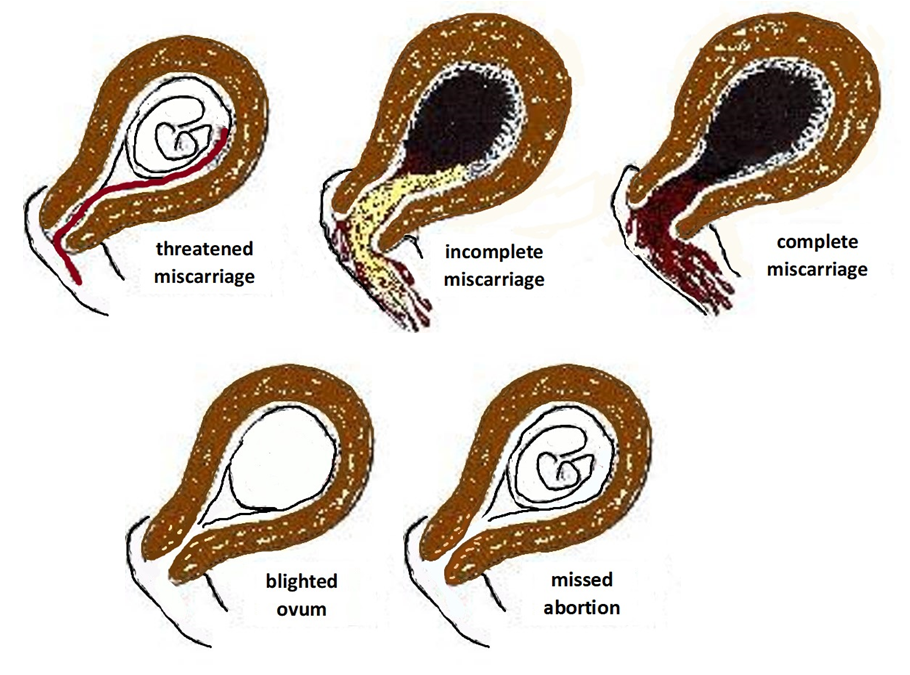
Classification of miscarriage
- A threatened miscarriage. When there is any amount of bleeding and your baby is still alive in your uterus then you are having what is called a threatened miscarriage. Often the bleeding settles and the pregnancy continues.
- An inevitable miscarriage is where there has been bleeding and the cervix has opened in preparation for miscarriage.
- An incomplete miscarriage is when some of the pregnancy tissue has been passed and some remains in the uterus
- A complete miscarriage is when all the pregnancy tissue has been passed.
- A missed abortion is where the baby has died in the womb but there is no miscarriage.
- A blighted ovum is where an empty pregnancy (gestational) sac seen on ultrasound scan.
- Recurrent miscarriage or habitual pregnancy loss is defined as three or more consecutive, spontaneous first-trimester pregnancy losses. When a woman has recurrent miscarriages of unknown cause the term idiopathic recurrent miscarriage is used.

Incidence of miscarriage
It is generally considered at least 20% of pregnancies end in miscarriage. The incidence is more as there are times a woman has a funny late period though without a positive pregnancy test it was not confirmed as due to miscarriage.
First-trimester miscarriage is much more common than a second-trimester miscarriage. The causes of first and second-trimester pregnancy losses usually are very different.
What are the causes of miscarriage?
These include:
- A chromosomal (karyotype) defect of the embryo (early foetus). The incidence increases with maternal age. Occasionally but not usually this is due to an inherited genetic trait from mother or father.
- Inadequate ovarian progesterone production. This is when the ovaries do not produce enough progesterone hormone for successful implantation and/or maintenance of the early pregnancy. Progesterone helps to prepare the lining of the uterus for implantation and creates a nutrient-rich environment for the developing baby.
- Maternal age. In the mid-30s this starts to become an issue, with the risk of foetal loss increasing with increasing age in late 30s and more markedly when a woman is in her 40s. There are multiple background factors why age can cause miscarriage.
- Uterine abnormalities. This includes an abnormal shape of the uterus and fibroids.
- Incompetent cervix. An incompetent or weak cervix may cause second-trimester miscarriages or premature labour.
- Polycystic Ovarian Syndrome. PCOS can cause difficulty conceiving as well as miscarriage.
- Other hormonal conditions. Poorly controlled diabetes and thyroid disease will increase the incidence of miscarriage.
- Autoimmune Disorders. Antibodies are designed to fight off infections in the human body. With certain autoimmune disorders, antibodies are present which fight off the developing pregnancy tissues, as if it is a foreign body or infection. Antiphospholipid syndrome (APS) is an autoimmune disorder diagnosed by blood tests that detect levels of anticardiolipin antibodies and lupus anticoagulant. Antibodies, such as anticardiolipin antibodies, can cause blood clots that clog up the blood supply to the placenta. Without the placenta supplying nutrients, the pregnancy will perish.
- Blood conditions. Certain inherited conditions mean that your blood may be more likely to clot than is usual. These conditions are known as thrombophilias. If you have a thrombophilia it can increase your risk of miscarriage.
- Uterine natural killer cells. uNK cells are the most numerous white blood cells found in the lining of the uterus that occurs during pregnancy (the decidua). Increased numbers of uNK cells can result in recurrent miscarriages.
- Infection. Infection can cause a miscarriage but is an uncommon cause of recurrent miscarriage.
- Multiple. It is possible to have more than one risk factor for miscarriage
- Unknown causes. Sometimes no cause for miscarriages is found. This does not mean there is no cause, but rather medical science today has not discovered all the reasons for miscarriage.
What can be done?
Management of miscarriage varies according to the situation and cause.
You should notify me if you have bleeding so I can work out what is happening and the correct management.
I will do an ultrasound scan to check your baby’s wellbeing. If a baby is well (threatened miscarriage) and you are in the first trimester of pregnancy I will usually arrange for you to have serial progesterone and quantitative HCG blood tests to help clarify and monitor the situation.
If you have a threatened miscarriage then rest and often progestogen pessary support is indicated. Progesterone pessaries can often prevent a miscarriage. I have had many patients who have seen me after multiple miscarriages and through using progestogen pessary support provided by me and close monitoring they have had successful pregnancies.
If you have an early pregnancy inevitable miscarriage or missed abortion then expectant management for a short time will suffice if this is your preference or else a curettage of the uterus can be done. The challenge is there is no way of determining how many days it will take before you miscarry.
With early pregnancy loss, the drug Misoprostol is a management option. Misoprostol is a medication that can bring on a miscarriage and so can avoid the alternatives of surgical or expectant management of miscarriage.
If after a period of time with an early pregnancy loss and expectant management hasn’t worked, or if Misoprostol hasn’t worked in causing a spontaneous miscarriage, or if you have an advanced pregnancy loss, or her an incomplete miscarriage, or if there is heavy bleeding or significant pain, or you want a curettage then I can do a curettage of your uterus to remove pregnancy tissue.
One advantage of a curettage is that I can send the pregnancy tissue obtained from your uterine cavity for checking for histology and chromosomes studies. This may indicate why the miscarriage happened, help you with “closure” and help with planning management of your next pregnancy.
If you have a complete miscarriage then nothing further needs to be done.
In all cases, your blood group will need to be checked and if you are Rhesus negative anti-D immunoglobulin needs to be given within 72 hours of bleeding.
Your next pregnancy planning and management will depend on what is the most suitable for you with consideration of what is the most likely cause for your miscarriage.
I have a special interest in the management of recurrent miscarriage and have been able to help many women have successful pregnancies who had before had multiple miscarriages.
I am able to offer a full range of treatment options including a vaginal progestogen therapy when inadequate ovary progesterone production appears to be the problem and oral prednisolone therapy when excessive uterine natural killer cells (uNK) seems to be the problem.
Also see our blog article Grieving after a miscarriage