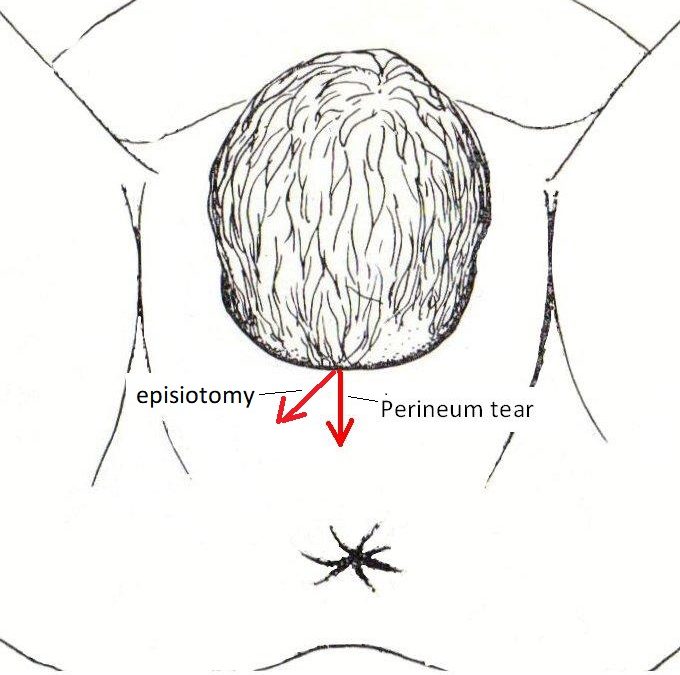
All women who have a vaginal delivery have the wish that their perineum will remain intact with the delivery of their baby. This is not always the case.  Many women experience perineal trauma with childbirth, either perineal tearing or an episiotomy or both.
Many women experience perineal trauma with childbirth, either perineal tearing or an episiotomy or both.
The most important determinants of whether there will be perineal trauma with childbirth and the severity of perineal trauma are…
- The elasticity of a woman’s perineal tissues. Some women’s perineums stretch very well and they can push out a > 4kg baby without any tearing. With some women, their perineum starts tearing even before the baby’s head is crowning. With some there is nasty tearing when the baby weighs <3kg.
- Whether there is prolonged pushing. Prolonged pushing often results in marked oedema of the tissues. Oedematous tissues are more likely to tear.
- The size of your baby especially of your baby and especially of your baby’s head.
- The position of your baby’s head (whether occipito–anterior or occipito-posterior as it comes out through the entrance of your birth canal). An occipito-posterior position is more likely to result in significant trauma as there is usually greater stretching of the perineum.
- Whether your baby’s head is well flexed or deflexed at delivery. A deflexed head means a bigger presenting diameter to deliver and more stretching of the perineum. This is common with an occipito–posterior position baby.
- Whether or not you have significant perineal scar tissue from a previous vaginal delivery. Scar tissue does not stretch as well and is more likely to tear.
- The competence and experience of your accoucheur. The accoucheur is the person delivering your baby.
- The speed and control of delivery of your baby’s head. A slow controlled delivery of baby’s head with a more gradual stretching of the perineum is more likely to result in no or minimal perineal trauma.
- Whether you have an epidural. An epidural is associated with a less perineal trauma as it results in a more controlled slower delivery of the baby’s head and not that sudden overwhelming to push hard because of pain. On the other hand, some women find it much harder to push their baby out with an epidural and end up with an operative vaginal delivery consequently.
- Your position at delivery. Delivering on “all fours” or on your side will mean there is less pressure on your perineum.
- Whether or not you push your baby out. If you have an operative vaginal delivery, then whether you have a vacuum delivery or a forceps delivery. There is less perineal trauma and often no perineal trauma with a vacuum delivery. This is because the suction cap is attached to the top of your baby’s head and does not increase the stretch of the perineum. Also, there is usually more control of delivery of the head allowing a slower and more controlled stretch of the perineum. For this reason, my preference is to use a vacuum cup for an operative vaginal delivery. I often have an intact perineum with a vacuum delivery. Forceps, in contrast, are applied to the sides of the head and so by using forceps there is a greater diameter and greater stretching of the perineum. Forceps use usually means an episiotomy is done to minimise perineal trauma.
- Women of Asian ethnicity are more likely to have significant perineum trauma and greater challenges with healing.
Severity of perineal trauma and suturing
If there is only minimal perineal trauma, then there is usually minimal discomfort after delivery and quick healing. If it is only grazing of the perineum, then stitches are often not needed.
If there is vaginal wall tearing and the perineum is intact then there is usually minimal (if any) discomfort, irrespective of the severity of the vaginal wall trauma.
With other than perineum grazing suturing to restore the perineal anatomy and facilitate healing is indicated. If the woman has an effective epidural, then no extra anaesthetic agents are needed. If she does not have an epidural or the epidural is not a good block, then local anaesthetic is needed before suturing. If she has sustained a 4th degree perineal tear, then usually it is repaired in the operating theatre under a general anaesthetic.
The amount of suturing required and the time taken to suture is proportional to the severity of perineal trauma. If there is more severe 2nd degree tear or a 3rd degree tear, then this is usually repaired with a woman’s legs being in stirrups and the doctor sitting in front of the perineum. This gives better access and optimises the ability to restore anatomy. If it is 1st degree tear or a less severe 2nd degree tear then the doctor will often suture while standing at the side of the woman with her knees flexed, legs apart at the knees and feet for access.
Pain relief after perineal trauma
If a woman sustains a more severe 2nd degree tear or a 3rd degree tear, then the doctor will usually offer to insert a Voltaren suppository into her rectum for pain relief. As well, the midwife will apply an ice pack to the perineum to help minimise discomfort and swelling.
The woman with be prescribed oral analgesics to be taken postnatally. How much analgesia is required is usually proportional to the severity of the trauma. Sometimes a woman with a low pain threshold or anxiety will need extra analgesia, even though she has sustained only minor trauma.
Particularly if there is more severe perineal trauma there can be perineal swelling usually on about day 3 postpartum. This will make the discomfort worse. The discomfort will also be worse if there has been perineal bruising. The midwife will check your perineum each day. If there is swelling or bruising, then further ice packs usually help with the discomfort.
Sometimes the discomfort is due to haemorrhoids and not to perineal trauma and its healing.
I suggest the use of ice packs be limited to if there is swelling or bruising and only be applied while in hospital and not at home. If the perineum is kept moist for too long then the skin softens and loses strength. That can result in the sutures pulling through and so resuturing is needed.
When you go home.
When you go home salt baths are a good idea to help with discomfort and healing. Place a cup of cooking salt in a low bath with the water temperature lukewarm. Soak your bottom in it for up to 10 minutes. You can do this 2-3 times per day. That will be soothing, reduce swelling and help with healing.
Otherwise keen your perineum clean and dry.
When you defaecate clean your anus area with toilet paper in the direction of your anus and away from your perineum. This held to prevent faecal soiling of your perineum. Then give your perineum a quick rinse and dry it with a hair blow dryer. You should do this until you are confident the perineum has healed. That will minimise the risk of infection and help with healing.
Minimise your activity the first week you are home from hospital. Excessive activity will put strain of your perineum and sutures and so the sutures are more likely to pull through.
Avoid constipation. You may need to take a stool softener. These can be purchased oner the counter in the chemist shop. They all work. Avoid red meat, junk food and fast food as these are often constipating. If you strain when you defaecate you will put more pressure on your stitches and so the stitches are more likely to pull through.
Sexual intercourse should be avoided until your perineum has fully healed and the lochia has ceased.
Very occasionally there is perineal breakdown. If it is very minor nothing needed to be done and the perineum will heal well. It there is more significant breakdown it is usually only the outer aspect of the tear or episiotomy and not full thickness. The perineum has usually been sutures with four layers of sutures. The perineum can usually be resutured in the office after cleaning and injecting local anaesthetic. Uncommonly is there a more major breakdown. If so or if the repeat suturing breaks down or if the patient is too anxious to allow resuturing in the office then resuturing can be done in the operating theatre under a general anaesthetic.
The most popular suture material is called Vicryl. It usually breaks down within two weeks. Sutures usually do not have to be removed.
The perineum is very resilient. Irrespective of the severity of trauma is usually heals very well. It has usually healed fully before your 6-week postnatal check-up.