On Friday I had four deliveries. In the afternoon at Norwest Hospital a patient in her first pregnancy had a normal delivery with an intact perineum. That evening at the San Hospital a patient in her first pregnancy had a normal delivery but needed an episiotomy. A student midwife was assisting me with delivery at the San Hospital. She asked me afterward: “How do you know when an episiotomy is needed?” That question has prompted me to do this article. It is a question of many patients.
What is an episiotomy?
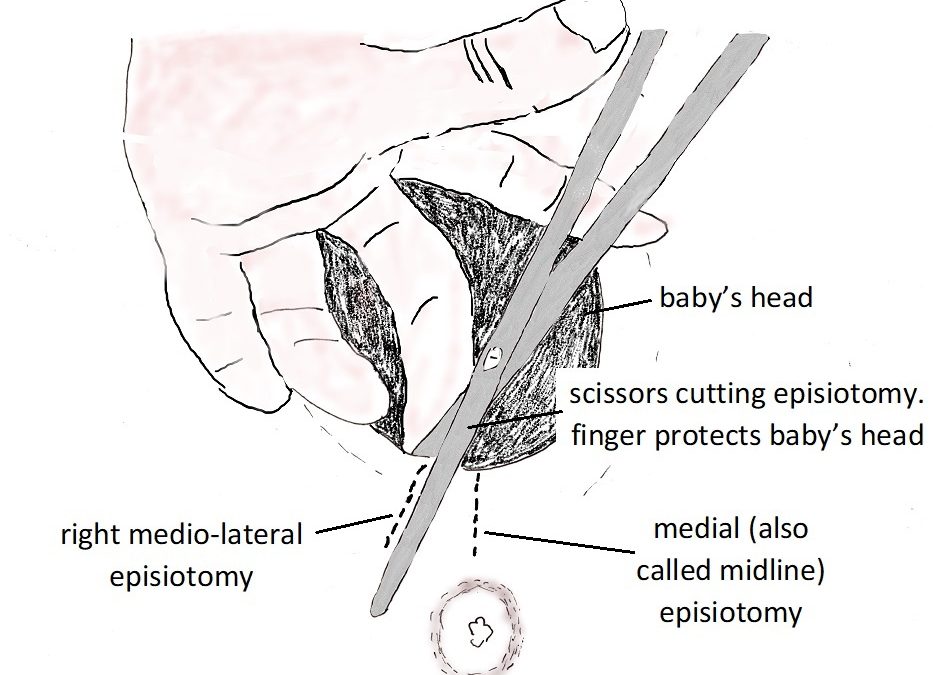
An episiotomy is a surgical cut of the perineum just before delivery of the baby’s head.
It can be medial (midline towards the anus) or mediolateral (starting midline in the perineum but cutting in a direction about 45 degrees to the midline and so away from the anus).
I always do a right mediolateral episiotomy. The direction is to the patient’s right is because I am right-handed. A mediolateral episiotomy is much safer as it aims away from perineal muscles, especially the anal sphincter. With a midline cut it can easily extend and so there is trauma to the anal sphincter.
Anaesthetic for episiotomy
If the labouring woman has an epidural block there is no need for a local anaesthesic when cutting the episiotomy or suturing afterwards. Occasionality the epidural is not sufficient for the episiotomy repair and so local anaesthetic is injected on the sides of the episiotomy cut before suturing. If no epidural, then local anaesthetic is injected in the line of the proposed cut prior to doing the episiotomy. Often extra local anaesthesic is needed so there is no pain with the episiotomy repair.
Why is an episiotomy done?
An episiotomy is done because there is increased risk of significant perineal tearing. Significant perineal tearing means there is increased risk of a large second-degree tear or a third- or fourth-degree perineal tear.
When is an episiotomy done?
An episiotomy is indicated when…
- Forceps delivery. The forceps blades are on either side of baby’s head and so results in greater stretching of the vaginal introitus (opening) and perineum with delivery and so increased risk of significant tearing. That is why I prefer doing a vacuum cup delivery to a forceps delivery when an operative vaginal delivery is needed. The vacuum cup attaches to the top of baby’s head and so there is no greater stretching of the perineum than usual. Often with a vacuum cup delivery there is no or minimal perineal trauma.
- Signs that a significant perineal tear is imminent when the baby’s head is crowning. These signs include oedema of the perineum, blanching (whitening) of the perineum, superficial perineum tearing and vaginal tearing. Oedema of fluid in the perineal tissues is due to a tight perineum. As well the tissue fluid results in a loss of strength of the tissues and so greater risk of significant tearing. Blanching is due to loss of blood flow into the perineum with stretching and is a sign that significant perineal tearing is imminent. Superficial tearing of the perineum is a sign the perineum does not have sufficient elasticity and will not adequately stretch with delivery. It is suggesting there will be significant tearing. A crucially concerning sign is when the superficial tearing occurs midway between the vaginal introitus and the anal sphincter. That is a sign of increased risk of third and fourth degree tearing.
- A perineum that is excessively tight and despite the woman’s best efforts at pushing is not stretching is at increased risk of sudden significant tearing.
- Previous third-degree tear. Some women who have sustained a 3a (partial tear of the external anal sphincter involving less than 50% thickness) request a vaginal delivery rather than Caesarean section. There is informed consent, so the woman understands the risk of further tearing of the anal sphincter the possible adverse implications of anal sphincter function. I also recommend an episiotomy so that perineal trauma is directed away from the anal sphincter and there is less likelihood of anal sphincter tearing.
- Breech vaginal delivery. While babies in breech presentation today are usually delivered by Caesarean section as it is a safer mode of delivery, if a breech vaginal delivery is done then an episiotomy is indicated to minimise the risk of baby’s head being trapped and being unable to be delivered.
An episiotomy is more likely to be needed when…
- Considerable scar tissue in perineum from previous delivery(ies). Scar tissue does not have the same elasticity as normal tissues and so is more likely to tear significantly. A minor amount of perineal scar tissue does not have the same risk.
- Occipito posterior (OP) position of baby’s head when crowning. An OP position means baby’s head is more deflexed, a greater head diameter is presenting and so there is greater risk of significant tearing. I have delivered women with babies in OP positions with intact perineums or only slight tearing, but there needs to be very careful assessment at the time because of the increased risk of significant tearing.
- Large baby. A large baby usually has a large head and broad shoulders. There is increased risk of significant perineal tearing and or shoulder dystocia (baby’s shoulders get stuck).
- Short perineum. Some women have a shorter distance between their perineum and anus and so if there is tearing it is more likely to involve the anal sphincter.
- Ethnic background. Many midwives have commented to me, and it is also my observation, that women of Asian background are more likely to sustain significant perineal trauma because of lack of elasticity of their perineal tissues.
- Extremely fit woman. Women who are very focused on physical activities and who are very fit can have very strong pelvic floor muscles and are unable to relax their pelvic floor muscles sufficiently for a vaginal delivery.
- Medical conditions. Occasionally a woman has a significant medical condition and has been advised by her doctor not to push or push excessively with delivery.
- An epidural is wonderful in that it gives a woman a pain-free labour. But the downside is that it makes it harder to push because of the loss of sensation to push. To get her to push just because she is in second stage labour will increase the likelihood of maternal exhaustion, lack of progress and an operative vaginal delivery. I am a great believer if baby is well in passive second stage so there is passive descent of the baby’s head to the perineum before she starts pushing. That increases the likelihood of a normal delivery and intact perineum.
- VBAC attempt. Excessive pushing is contraindicated as there is increased risk of uterine rupture.
Will I need an episiotomy next time?
If a woman has had her first baby vaginally with no or minimal trauma then it is likely she will have subsequent babies with minimal or no trauma to the perineum, and so no need for an episiotomy.
If an episiotomy was done first time, then there is increased likelihood of a second delivery episiotomy. The indication for the episiotomy with the first delivery may be relevant for her second delivery. As well there is perineal scar tissue, with less elasticity.
Many women who had an episiotomy first time do not require an episiotomy with subsequent deliveries. There needs to be careful guarding of the perineum and very slow controlled delivery of baby’s head. I have managed many women who had episiotomies with their first deliveries and then had intact perineums or only small perineal tears.