It was Mother’s Day. The plan was to have a celebration breakfast wife my wife Robyn, give Robyn her Mothers Days gifts, then go to church with Robyn, then lunch and then take Robyn to our daughter’s home for a Mothers Day celebration afternoon tea with all the family.
When I was getting ready for church when my phone went. It was the Birth Unit. The midwife advised me that a patient had just arrived in labour. She was 39 weeks and 6 days pregnant. She was 6cm cervical dilatation. She wanted an epidural.
This patient was a wonderful person in her first pregnancy. She chose for me to continue her pregnancy care after she moved from interstate to Sydney with her husband to live at 32 weeks pregnancy. Gestational diabetes had been diagnosed which had been managed well with diet changes alone. No insulin was required. Otherwise her pregnancy was uncomplicated.
Her baby’s head had been engaged in her pelvis from 37 weeks pregnancy and the baby was of appropriate size for dates on ultrasound scans I did at each antenatal visit.
At her 39 week pregnancy visit she said that she was keen to be induced. Her husband had just arrived from working interstate. He only had a limited time off work in Sydney until he had to go back to work interstate. As well there was the gestational diabetes and so I did not want her to go too much overdue. I did an internal examination to assess her suitability for induction. Her cervix was 3cm dilated, 1.5cm long, soft and the baby’s head was well applied to the cervix and at station –2. I advised her that her cervix was very favourable for induction and I anticipated she would have a good labour. I did a cervical stretch and membranes strip in the hope that this would put her into labour and so the induction would not be necessary. I booked her induction for the following Monday. She came in in labour the day prior.
After speaking to the midwife I went to church. At the end of the church service I phoned the hospital. The midwife said the patient had an epidural and she did an ARM and there was clear liquor. She said that the patient was now fully dilated. She was soon going to ask her to start pushing. As I expected she had a good first stage labour with good progress. The baby’s well-being was assessed by the CTG (cardiotocogram or continuous foetal heart rate monitoring) was good, with a normal foetal heart rate pattern. I said I did not want her pushing too soon with the epidural working and would like the baby’s head to descend passively as much as possible, as long as baby was ok and the epidural was effective re pain relief. This was to minimise the likelihood of needing to do an operative vaginal delivery. If a patient starts pushing too soon with an epidural working the pushing is often less effective and there can be lack of progress and maternal exhaustion.
I went home from church. No sooner had I arrived home when I received a call from the midwife. She asked if I was on my way to the hospital yet. I said no. She said I had better come as she did now not like to look of the baby’s CTG. I went to the hospital immediately.
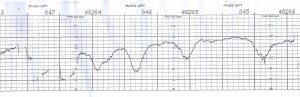 When I arrived I studied the CTG and agreed it was very concerning. It had suddenly changed from normal foetal heart trace pattern to a very abnormal trace consistent with the baby now experiencing reduced oxygenation (called ‘asphyxia’). The baseline heart rate had increased to an abnormally high level, there was loss of the normal ‘up and down’variations of the heart rate pattern (called variability) and there were large late (timing onset in relation to the contraction) decelerations (episodes of slowing) of the baby’s heart rate.
When I arrived I studied the CTG and agreed it was very concerning. It had suddenly changed from normal foetal heart trace pattern to a very abnormal trace consistent with the baby now experiencing reduced oxygenation (called ‘asphyxia’). The baseline heart rate had increased to an abnormally high level, there was loss of the normal ‘up and down’variations of the heart rate pattern (called variability) and there were large late (timing onset in relation to the contraction) decelerations (episodes of slowing) of the baby’s heart rate.
I discussed the situation in detail with the patient and her husband and said that her baby needed urgent delivery. I did an internal examination and confirmed that her cervix was fully dilated and the baby’s head was well engaged and had descended to midway down the lower half of her birth canal. There was now staining of liquor with fresh meconium. This was another concerning sign of foetal distress.
We placed her legs in stirrups for a vacuum delivery. After putting her in stirrups and before I had time to apply the suction cup to the baby’s head she had a contraction. I asked her to push with this contraction. She did amazingly well and pushed the baby’s head down the birth canal and onto her perineum so it was ‘on view’. In view of this incredible effort and excellent progress I waited until the next contraction and encouraged her to push again. This she did and had a normal vaginal delivery with only a first degree perineal tear.
Her daughter was born in excellent condition and had a birth weight of 3614gms. Her baby was well aspirated in view of the meconium stained liquor but did not need any resuscitation. The umbilical cord was below the shoulder but not tight. There was no other obvious cause for the foetal distress.
I then went home for a late lunch with my wife. We still got to my daughter’s home for a Mothers Day celebration afternoon tea with all the family.
Postnatally mother and baby both did well and both have been discharged home. Mum is successfully breastfeeding her baby.
This patient’s labour and delivery highlight how quickly and how dramatically foetal well-being can change in labour. It also illustrates how important it is to be diligent in labour management, provide good quality care and have a compliant patient to underpin a good outcome. Without this the outcome for her baby could have been very different.

