What is labour?
 First stage labour is defined as regular coordinated contractions that cause your cervix to dilate. The onset of labour is when your contractions cause this to happen. There may be increased uterine activity in the days or even weeks before true labour starts. This can cause confusion in knowing the time of the onset of actual labour.
First stage labour is defined as regular coordinated contractions that cause your cervix to dilate. The onset of labour is when your contractions cause this to happen. There may be increased uterine activity in the days or even weeks before true labour starts. This can cause confusion in knowing the time of the onset of actual labour.- Second stage labour starts when your cervix is fully dilated (10cm). This is the time you are encouraged to push and deliver your baby.
- Third stage labour starts after your baby is delivered and ends when your placenta is delivered.
When does labour happen?
 Labour usually happens at term gestation, which between 37 and 42 weeks pregnancy. If its onset is before 37 weeks it is called pre-term labour. After 42 weeks you are post-term.
Labour usually happens at term gestation, which between 37 and 42 weeks pregnancy. If its onset is before 37 weeks it is called pre-term labour. After 42 weeks you are post-term.
How do I know I am in labour?
- You will become aware of regular contractions of increasing frequency and severity. For most women you should call the Labour Ward / Birth Unit midwife when aware and she will usually advise you to come to the hospital when the contractions are five to 10 minutes apart. Also contact your husband / partner to come home and start organising care for children you have. Some woman want to stay home longer as there are no risk factors that mean they should attend the hospital at this stage and they are coping. That’s ok! Just don’t get caught out where you go from “I am coping” to “I want to push” and you are still at home!
- Labour can be heralded by a show (mucus streaked with blood from the vagina), though this sometimes may occur days before labour starts. If blood loss is more that this phone the hospital immediately.
- Sometimes there is spontaneous rupture of the membranes before the onset of labour, though usually this happens the other way round. If this happens contact the hospital.
What happens at the hospital?
 You will be greeted by the midwife assigned to you.
You will be greeted by the midwife assigned to you.
She will interview you about what is happening, about your pregnancy to date, your past obstetric history and about your labour and delivery preferences. Make sure you bring your antenatal card to show her.
She will check your ‘obs’ – temperature, pulse and blood pressure and may want to check your urine. She will palpate your abdomen and check your baby’s position and whether there is engagement of your baby’s head in your pelvis.
She will then want to monitor your baby’s well being and your contractions with a CTG (cardiotocogram). This can be discontinued after about 30 minutes if all is well and there is no reason to continue the monitoring.
You will have an internal examination done by the midwife unless this is contraindicated for some reason (eg. low placenta or preterm labour).
Once this is done I will be contacted and informed.
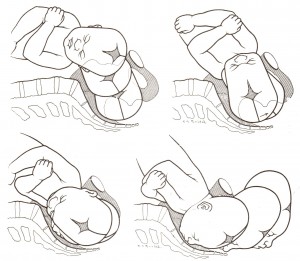
There will periodic checks of your ‘obs’, your baby’s well being (foetal heart auscultation or CTG) and internal examinations in labour to assess your progress in labour. With these internal examinations you will be checked for how dilated your cervix is, how thick your cervix is, how low your baby’s head is in the pelvis and as you progress the way your baby’s head is turned.
The midwife will give me regular updates of your progress. Your progress in labour is recorded on a labour ward chart in your notes or on the monitor called a ‘partogram’. There is an accepted normal rate of progress in labour. It should be at least 1cm/hour first labour and 1.5 cm/hour subsequent labours.
If your progress is suboptimal the reasons will be considered. Often rupturing of your membranes (if this hasn’t happened) and possibly also a Syntocinon intravenous infusion will be suggested to accelerate labour. If despite these measures there still suboptimal or sometimes even no progress in labour in first stage labour then a Caesarean section will be considered because it is likely your baby is too big for your birth canal. This is called an obstructed labour or cephalo-pelvic disproportion.
When you are in second stage labour the midwife will encourage you to start to push your baby out. The timing of the onset of pushing in second stage will vary.
If all goes well you will be able to push your baby out. You will have had a normal or spontaneous vaginal delivery.
If there is lack of progress in second stage labour despite your best maternal effort and optimal contractions you may need an operative vaginal delivery. This will usually be with vacuum device. I am also highly skilled with the use of forceps and in some circumstances forceps may be the more suitable option. I have noticed most obstetricians starting out now have little or no experience in forceps and so do not have the same skill set and confidence with operative vaginal deliveries. Occasionally a Caesarean section is needed despite being in second stage labour. This is because is clear that an operative vaginal delivery has too much risk for your baby.
From delivery on the baby until after the placenta is delivered is called third stage labour. This is usually quite quick. The placenta separates from the uterine wall and is delivered by controlled cord traction. Occasionally it doesn’t separate and so is retained and a manual removal of placenta is needed with a suitable anaesthetic.
Also see:
- Labour and Delivery in the Pregnancy Care section
- Vacuum and Forceps in the Questions and Answer section

